A herniated disc is often called many terms with important specificity; however, for the simplistic purposes of general education, you may hear the terms: bulged disc, ruptured disc, torn disc, etc. Herniated disc treatments typically involve physical therapy exercises, chiropractic care, massage therapy, distraction therapy, and various forms. However, the best herniated disc treatment will be the one that quickly reduces pain. We find McKenzie Therapy to be the type of treatment and exercises that patients with herniated disc(s) need to find relief today. A herniated disc most commonly occurs in the low back; however, it may happen at any region in the spine affecting or not affecting nearby nerves that exit the spine. These discs are closely positioned to nerve roots.
The Human Spine Consists 23 Intervertebral Discs
-
6 in the neck (cervical region)
-
12 in the midback (thoracic region)
-
5 in the lower back (lumbar region)
The Human Spine Consists of 31 Pairs (62 total) of Nerve Roots.
-
8 pairs (16 total) in the neck (cervical region)
-
12 pairs (24 total) in the mid back (thoracic region)
-
5 pairs (10 total) in the low back (lumbar region)
-
5 pairs (10 total) in the tailbone (sacral region)
-
1 pair (2 total) in the utmost lowest part of the tailbone (coccyx region)
Already, this appears to be intimidating. You can be assured the human body is very resilient and adaptable. The discs serve a large purpose in shock absorption whether sitting, standing, walking, running, or exercising; you place a reflected amount of force onto the disc to protect the spine and spinal cord. The spinal cord lives within the spinal canal with nerve roots exiting the spinal cord from foramen made from the adjacent vertebrae.
HERNIATION
The disc is made up of two main components: an annulus fibrosis and a nucleus pulposus. The annulus fibrosis is a very tough dense ring-like structure encasing the nucleus pulposus. The nucleus pulposus is a soft, jelly-like material that resides in the center of the disc. A herniated disc occurs when the annulus fibrosis experiences a tear. This tear allows for the jelly-like material to escape the center of the disc and leak outwardly potentially affecting associated nerve roots, most commonly producing sciatica.
The tear to the annulus fibrosis can occur from significant trauma or poor repetitive loading strategies (“wear and tear”) compounded from daily activities & posturing. Most commonly, disc herniations are seen on MRI’s with mechanisms of injury resulting from “no apparent reason”, therefore, attributing the herniation to “wear and tear”. The risk factors associated for herniated disc(s) include improper lifting, weight, repetitive activities that place strain on the spine, prolonged sitting, sedentary lifestyle, and smoking is believed to lead to a more rapid degeneration.
SYMPTOMS
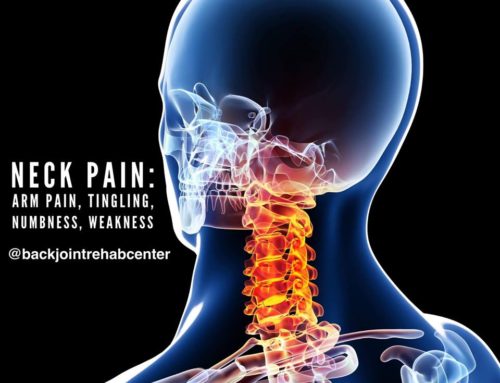
The onset of symptoms typically associated with a disc herniation is low back pain. This presentation can worsen as the disc begins to irritate or compress the associated nerve root on either side or both. This will result in radiculopathy which means that a specific nerve is affected producing symptoms of pain, weakness, numbness, or difficulty controlling muscles.
Sciatica is the most popular name amongst nerve conditions. It implies the nerve roots that make up the sciatic nerve are irritated or compressed, most likely due to a disc herniation, sending pain or other associated symptoms. The frequency and intensity of pain are commonly varied. While red flags present an immediate surgical intervention; they are not common, but consist of: loss of bladder or bowel control. This is called Cauda Equina Syndrome. If you experience loss of bladder or bowel control, please call 911 and visit your nearest emergency hospital.
IMAGING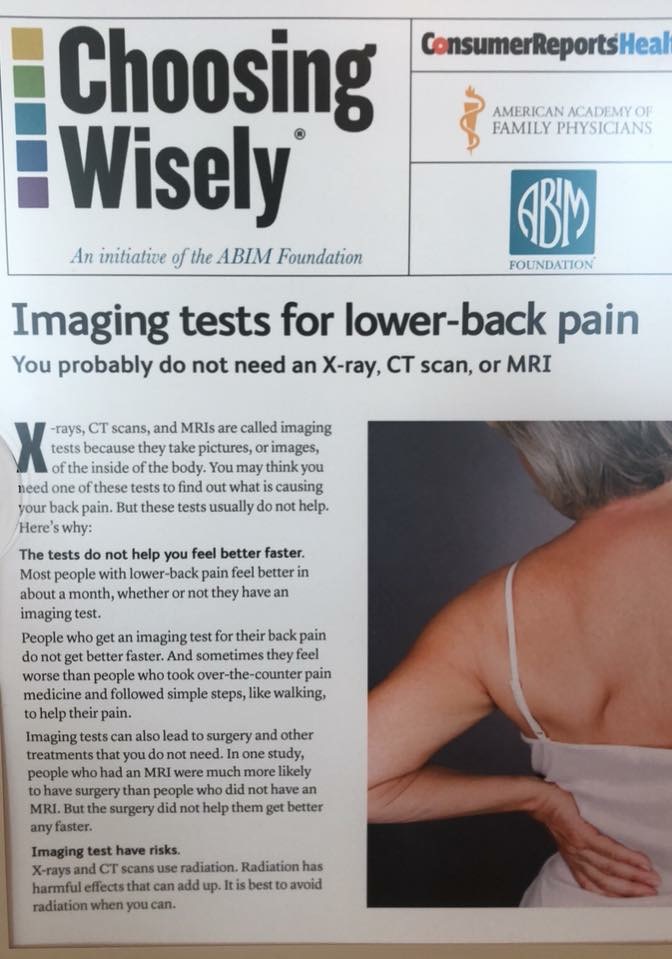
A disc herniation can only be confirmed with an MRI or CT; however, patient history and physical examination can lead to a strong inclination of the presence of a disc herniation; keep in mind it’s confirmation can only be made with the appropriate diagnostic image. An MRI is most commonly preferred. An X-Ray CANNOT confirm a disc herniation. While an MRI confirms the presence of a disc herniation in the case where you have symptoms; the research demonstrates a significant presence of spinal degeneration and disc herniations in populations who do not feel symptoms. This leaves the impression that spinal abnormalities found on imaging should not be the primary factor utilized in clinical decision making for your course of treatment or care. The diagnostic imaging should be utilized to confirm the presentation, examination, and concluded prognosis. Together, this will guide the appropriate course of action.
TREATMENT
First course of care is typically non-surgical. Majority of cases can improve over a course of 6-16 weeks while experiencing episodes during their recovery. The most common misconception is that the disc herniations require surgery. Most cases do not require surgery and can be resolved with spinal rehabilitation. At times, a combined approach of pain medication or spinal injection with rehabilitation is necessary during significant amount of constant pain.
Considerations for surgical intervention is taken into account when conservative care has not improved the patient’s condition, the condition has rapidly worsened, the development of red flags has occurred, or in small populations